how ai is battling one of our worst, least talked about global crises
Bacteria are rapidly evolving resistance to more, and higher doses of our most reliable antibiotics, but AI can help us avoid a catastrophe.
One of the worst things about the current AI craze in the media and Silicon Valley is that the focus so far has been on, well, some of the worst possible uses for the new technology. We can’t stop hearing about ChatGPT and what author John Scalzi very appropriately called art-barf robots, and how they’re about to make doctors, lawyers, engineers, and hell, everyone obsolete. But we seldom hear about genuinely positive uses for AI.
To be fair, a big part of the reason why are the people trying to sell AI in the first place. OpenAI’s CEO Sam Altman is demanding $7 trillion — which is almost every tax dollar collected at every level in the United States per year — to build a“superhuman AGI” that will then tell him how to make money on it. It’s an utterly demented proposition for reasons I need a dedicated post to explain, but it gets a lot of attention and sucks the oxygen out of the room for truly interesting things we’re doing with AI.
For example, chat bots can help us make small but very sustainable and meaningful lifestyle changes by reminding us to eat better and move around more with inhuman patience and positivity. They’ve nailed down the customer service voice anyone who worked in retail knows all too well, and that lets them give people the feeling of being heard, which allows specially trained chat bots to fight disinformation with unfailingly polite nudges. (Although that ability is a double edged sword because it could be used the exact opposite way just as effectively.)
Likewise, AI is getting really good at reading certain types of medical imaging and can help doctors pay more attention to scans that may have otherwise slipped by as false negatives, flagging depression and anxiety, and helps patients with severe disabilities requiring implants interact with the world more authentically and independently. It’s even helping physicists understand the fundamental laws of the universe.
Better still, AI is quietly tackling one of the biggest and thorniest problems we should be hearing a lot more about but don’t: antibiotic resistance.
how a magic pill backfired on us
When penicillin was discovered, it was one of the most profound medical advances ever, on par with vaccines. Suddenly, a cut that wasn’t treated with outmost vigilance wouldn’t be a death sentence. Surgeries became infinitely safer. Hospitals in general were now far better equipped to stop the spread of infections and treat their patients before problems from bacterial colonizations and diseases became unbearable and way too difficult to manage effectively.
As an added bonus, antibiotics also made sex safer, as they easily treated a number of once endemic infections. Syphilis served as the inspiration for modern zombies as the afflicted shambled through alleyways, their brains being eaten alive, noses, ears, and lips falling off in the advanced stages of the disease. With antibiotics, there were now far fewer Walking Horny Dead.
Yet, we took this great thing and managed to fuck it up, and fuck it up badly. You see, bacteria reproduce very quickly. We like to say that creatures are breeding like rabbits when we mean they’re prolific. But even rabbit reproduction takes tens of millennia compared to microbes, as you get five to seven bunnies in a month and the doubling of an entire microbial population in 4 to 20 minutes.
Just imagine an entity the size of a small solar system getting pregnant at the dawn of the agricultural revolution and the construction of the first temples, then finally giving birth sometime this year, and you’ve now placed yourself firmly in a bacterium’s shoes looking at rabbits multiplying. (You may need to buy those shoes in bulk because you may have up to a few hundred flagella that need covering.)
“But hold on, don’t bacteria just duplicate themselves? They don’t mix genes like us sexually reproducing organisms, so all that could happen is more copies of the same microbes. How problematic could a bunch of clones we know how to kill be?”
Well, the duplication process is not without its flaws and the nucleobases which form the helix of their DNA or RNA don’t always replicate one to one, leading to what we’d call typos in its clone’s genetic alphabet. A bunch of these mutations are deleterious, a lot of them do nothing, but some offer an advantage in the right environment. Put a bacterium with the right mutation under the right selective pressure and they evolve to deal with it after thousands of generations in the span of a few months. (All of this has been beautifully demonstrated in a long running experiment that had creationists losing their shit in rage.)
If that environment is full of antibiotics, there’s now a much higher chance for these bacteria to develop mutations that let them counter their effects, so more and more bacteria will eventually become resistant, if not immune. They don’t have a choice. If they don’t inherit resistance or develop new pathways for it, they’ll die off.
And thanks to massive, unnecessary, preemptive and sometimes defiant overuse of antibiotics on farms, doctors in far too many nations dispensing them like candy for every cough or sniffle, and patients neglecting to finish their courses as soon as they feel better, we keep pressuring more and more bacteria to evolve resistance.
making resistance futile again
If we no longer have an arsenal of reliable antibiotics, surgeries will again become a dangerous affair, and many won’t even happen due to fear of infection. Old and new bacterial infections will soar once again. Even tooth extractions will become an ordeal, and meat from factory farm animals will be responsible for more food-borne illnesses than it has been in a nearly a century, and with more complications than ever before. Not to mention that STDs we thought we defeated will come roaring back and cause long term damage, a threat we recently faced with gonorrhea.
I say faced because we got lucky. We discovered a new antibiotic called zoliflodacin, which attacks the responsible bacteria in a novel way, biochemically outflanking the germs. But that means we have a decade or two before we need to be working on a new way to fight the same germs because they will evolve resistance to it since there will be literally a million chances for them to wander into it.
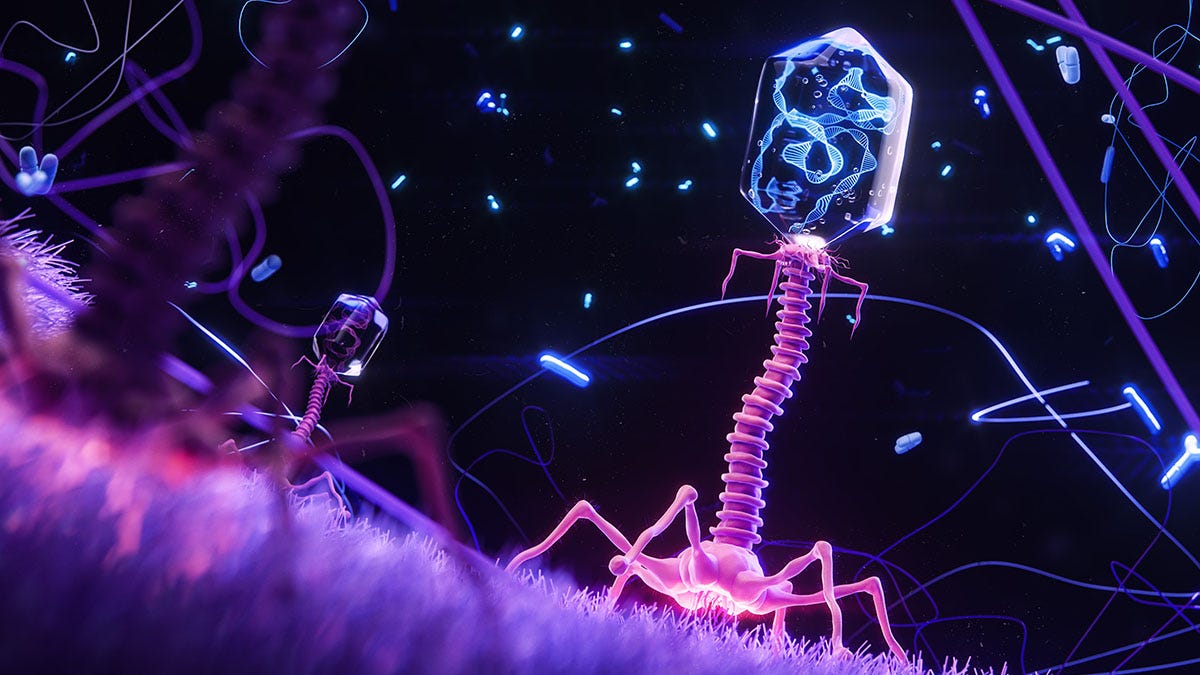
Broadly, there are four ways we can fight this problem. First, we can really put our foot down and reign in antibiotic overuse on farms and in doctors’ offices. Second, we can find alternative treatment methods like custom cocktails of bacteriophages, a group of viruses which attack specific bacteria we want gone, blended into an IV. Third, we find new ways to use existing medical treatments to bypass bacterial resistance. And finally, we can just keep discovering new antibiotic compounds faster than resistance fully evolves and becomes a problem again.
The first method is a massive political, regulatory, and educational undertaking that is well underway, and where we will need to succeed to give ourselves more breathing room by releasing the selective pressure on bacteria, but will take many years to pay off. Far too many people are used to the idea that if they pop the magic pills, all their sickness goes away — even if it was a virus and was going to go away on its own — their livestock gets bigger, fatter, and has fewer infections, and it feels like there are no side effects, even as bigger doses and longer courses to fight these germs wreck the gut flora of billions.
The second method is expensive, complicated, and uncertain because it requires special treatments customized for each patient’s strain. Not every phage will attack every bacteria. Each has its own way of attacking its targets, and doesn’t always kill the microbe it infects. There are some promising experiments, and phages evolve to keep up with their prey, but we don’t know how sustainable this would be in the long term because the appropriate research is just starting.
And as for the last two methods, the problem space is so vast, it would take scientists many decades to find the right molecules through trial and error. But you know what’s really good at navigating a vast problem space with billions of possible solutions and brute forcing their way to the right answers? Computers.
better living through automated biochemistry
“You know what this reminds me of? The phase where all those crypto bros on social media replied to literally everything people were complaining about with ‘bitcoin fixes this’ even if it was someone with appendicitis.”
Okay, yes, I hear you. But there’s a big difference. Crypto, as a whole, is a solution in search of a problem because its creation story is basically people saying “you know, I really hate those fucking banks, both retail and central, so I’m gonna invent my own money!” even though for almost everyone, modern money works fine. (And in some cases, it was actually more “you know, I really hate those money-grubbing Jews,” but that’s another topic for a future post.)
But when it comes to antibiotic resistance, AI can absolutely help because it can use the fundamental rules of biochemistry to either identify molecules that can bypass a microbe’s resistance to certain antibiotics, or look at the processes keeping it alive or fit enough to reproduce, then suggest potential new antibiotic compounds which will interfere with its biochemical machinery. It’s fundamentally the same thing any human researcher does, just millions of times faster, and with a built in fact check to see how likely its suggestions are to work before even offering them.
Even better, well designed algorithms can group together various compounds flagged as potentially promising in the fight against certain bacteria and their chemical family, giving researchers new ideas and avenues to test the same way. For example, one of these AIs found that an anti-parasitic called triclabendazole also happened to target a critical protein keeping certain bacteria alive, and the same applied to drugs used for other parasites, anxiety, and cancer.
In other words, it helped identify non-antibiotics that can be used to combat ordinarily resistant bacteria by registering that these drugs’ active ingredients also happened to interfere with key proteins and their synthesis in the target bacteria. Could humans do something like that? Sure. In fact they did by specifying the line of inquiry for the AI to pursue. But the AI just took over to vet 2 million potential ways 200 drugs could kill a bunch of mutant E. coli bacteria in a matter of days rather than months or years, then map the results in a way that let researchers see even more possibilities.
Another AI developed by MIT used a more targeted approach to identify a whole new class of nearly 300 antibiotic compounds when asked to consider how well 39,312 candidates would do against methicillin-resistant MRSA. Lab experiments backed up the model’s conclusions, reducing bacterial colonies by at least 90%. Of course, it’s not impressive if the model could only handle one target, so it doesn’t. You can feed it a library of chemical compounds, give it any target, and it will spit out another class of antibiotics if they exist.
Not to let that be a limitation, there’s work on other AI models that can discover a new compound by testing what molecules could be synthesized or combined into a stable structure. If you’re wondering whether they can be hijacked to synthesize all sorts of horrible bioweapons, the answer is that they can, but that can also design antidotes to those bioweapons on the fly, so, you know, exercise caution with them if you’d rather not become an accidental Bond villain or doomsday cult leader.
While antibiotic resistance will always be a thing and we need to stay on top of it, stop using them willy-nilly in farms and for the sniffles, and cut down on doses we give out as there are serious side-effects to antibiotic overuse, these AIs give us hope that it’s possible to invent our way out of this looming crisis and stay one step ahead of even the wiliest, fastest evolving bacteria. And that’s the kind of AI use case to which there needs to be a whole lot more media attention than to paper-pushing chat bots and the grandiose dreams of tech VCs who want to colonize the solar system.
See: Noto Guillen, M et al. (2024) Antibacterial activity of nonantibiotics is orthogonal to standard antibiotics, Science 384, 93-100, DOI:10.1126/science.adk7368
Wong, F. et al. (2024) Discovery of a structural class of antibiotics with explainable deep learning. Nature 626, 177–185, DOI 10.1038/s41586-023-06887-8
![[ world of weird things ]](https://substackcdn.com/image/fetch/$s_!V-uR!,w_80,h_80,c_fill,f_auto,q_auto:good,fl_progressive:steep,g_auto/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F93728edf-9a13-4b2b-9a33-3ef171b5c8d8_600x600.png)